Identifying nursing interventions captured in patients with stroke by Korean nursing students: Nursing interventions classification study
Article information
Abstract
Purpose
This study aimed to identify nursing interventions captured in patients with stroke by Korean nursing students for the categorization of nursing care tailored to the characteristics of stroke patients.
Methods
To identify nursing interventions, a descriptive data analysis was conducted using case scenarios written by nursing students during clinical practice in rehabilitation care settings. The case scenarios were analyzed using the standard terminology classification system, nursing interventions classification (NIC), to identify and categorize interventions for patients with stroke.
Results
As the result of analysis, we identified 10 most frequent NIC interventions. The most frequent NIC intervention was vital signs monitoring (N=244, 8.6%). The 89 nursing interventions were classified into 7 domains and 24 classes of the NIC system.
Conclusion
The results of this study can be used as a basis for a list of nursing interventions tailored to the characteristics of patients with stroke and furthermore calculating nursing fees through the analysis of nursing interventions for these patients.
INTRODUCTION
Stroke is still the main cause of death following by cancer and heart disease in Korea due to an increase in major causes such as hypertension, diabetes, obesity, hyperlipidemia, and heart disease [1,2]. Once a stroke occurs, most patients have various types of disabilities such as loss of motor, paresthesia, cognition, and language, depending on the brain lesion. These dysfunctions interfere with the patient's independent performance of daily activities. As a result, patients experience deterioration of activity, damage of autonomy, interpersonal relationship problem, leading to long-term depression, anxiety, and psychosocial maladjustment [3,4].
For stroke patients, early systematic rehabilitation treatment is very important, and effective coping has a significant impact on returning to social life. In terms of the nature of stroke requiring long-term care, it is necessary to improve the capacity to maintain a physically independent daily life as much as possible, and requires specific care. In particular, nursing intervention could be help patients cope appropriately with physiological or psychological problems caused by a changed life-style and social prejudice after stroke [4-6].
The goals and the content of nursing interventions also should be changed as the disease progresses. Nurses should provide the accurate and appropriate nursing intervention with the perspective to look at various problems in an integrated manner. These competencies should be trained from the time of nursing students experiencing clinical practice, and there is a need to educate and improve the competency to select an integrated and accurate interventions for patients. The improvement of competency begins with the use of standardized nursing interventions in clinical practice [6-8].
Therefore, it is necessary to try categorization of nursing interventions specific to stroke patients through case analysis written by nursing students, and this analysis will be essential for establishing standardized interventions for cardiovascular care. However, to date, Nursing Interventions Classification (NIC) studies on stroke are insufficient. In previous studies, validity and reliability analysis of some of NIC (e.g., self-care assistance) [9], single patient case [10], thrombolytic patients [11], post-discharge interventions [12], acute and subacute interventions [13] were nurses, cerebral hemorrhage [14] was nursing students, but it is difficult to find recent studies.
Thus, this study aimed to identify and categorize the most prevalent nursing interventions for patients with stroke selected by Korean nursing students according to the NIC system during clinical training in rehabilitation care settings.
METHODS
1. Research Design
This was a retrospective research using the NIC system to identify and categorize the nursing interventions captured in the case scenarios submitted between March 2018 and December 2019. The case scenarios were written by Korean nursing students who were in the fourth year and had completed the adult nursing unit training.
2. Data Collection and Analysis
The data were collected from 142 scenarios about patients with stroke submitted by fourth graders Korean nursing students of K University who had done 8 weeks of clinical training in a general hospital. Data were verified by two experts with terminology research experience, more than 10 years of clinical career, and doctoral degrees in nursing. The reliability between the experts was 81.6%. Moreover, we selected nursing interventions with content validity index (CVI) of 0.60 or higher. Nursing interventions can be recorded more than one according to the symptom or condition of a patient, and any nursing activity or behavior provided to the patient may also be recorded as an intervention. Among the interventions, if they could not be described as NIC interventions, they were linked to appropriate NIC interventions and then analyzed. Incomplete or ambiguous nursing interventions were excluded before analysis.
Data analysis was performed using Microsoft Access and Excel (Microsoft, Redmond, WA, USA). We inputted extracted data (demographic and clinical information of patients, the label, definition, domain, and class of NIC) into the Microsoft Access. We calculated the number, percentage, and prevalence of NIC interventions.
3. Nursing Interventions Classification
Nursing interventions are behaviors performed based on nurses' clinical decision and scientific knowledge to improve patient outcomes. We used NIC system developed by the research team at Iowa University, United States to identify and categorize nursing interventions. The NIC system is classified into 3 levels, 7 domains, 30 classes, and 565 nursing interventions. The 3 levels are: domain, class, and intervention. The 7 domains (physiological: basic, physiological: complex, behavioral, safety, family, health system, and community) are classified into 30 classes. Each intervention is listed with a code, a label, activities to achieve the intervention, and literature. NIC supports an evidence-based practice tool to help nurses provide specific interventions, and standardizes the nursing knowledge. Investigating the concept of nursing interventions is a basic process of establishing the essence of nursing, systematizing the professionalism and independence of nursing knowledge [15,16].
4. Ethical Considerations
This research was approved by the institutional ethics committee of the K university (No.: 2022-0157). The patients scenarios written by nursing students for analysis were used in this research after deletion of personal information. The committee also approved the withdrawal of consent to use the data.
RESULTS
Ethics statement: This study was approved by the Institutional Review Board (IRB) at K university (approval No.: 2022-0157). The case scenarios written by nursing students for analysis were used in this study after deletion of personally identifiable information. The IRB also approved the waiver of consent to access this data.
1. Demographic Characteristics of Stroke Patients
Of a total of 142 patients with stroke, 76 (53.5%) were female. The mean age of the patients was 65.4 years, most of them were older than 65 years of age (n=89, 62.7%). The majority (n=135, 95.1%) of the patients had an education level of elementary school or higher, and most of them were unemployed (n=108, 76.1%). As for the type of residence, the majority (n=97, 68.3%) lived with someone else, most often their spouse (n=72, 50.7%). Approximately 89 of patients had above the upper middle economic level (62.7%), and 36 of patients were smokers (25.4%) (Table 1).
2. Clinical Characteristics of Stroke Patients
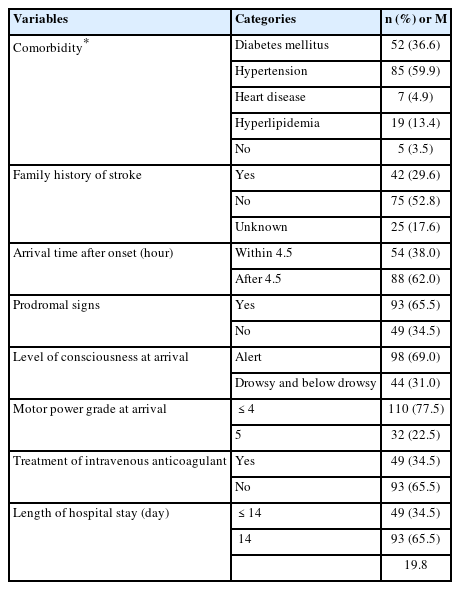
The majority (n=137, 96.4%) of patients had comorbidities in the order of hypertension (n=85, 59.9%), diabetes mellitus (n=52, 36.6%), hyperlipidemia (n=19, 13.4%), and heart disease (n=7, 4.9%). Only 42 (29.6%) patients had family history of stroke. Fifty four (38.0%) patients arrived within 4.5 hours after onset. Ninety-three patients (65.5%) had prodromal signs, 98 (69.0%) had an alert level of consciousness, and 110 (77.5%) had 4 points or less of motor power grade. Only 49 (34.5%) patients received intravenous anticoagulant, and the mean length of stay in the hospital was 19.8 days (Table 2).
3. NIC Interventions for Patients with Stroke
A total of 89 interventions were identified in the scenario, and these interventions were distributed in 7 domains and 24 classes. Table 3 shows top 10 NIC interventions, as well as the domains and classes to which they belong. Of the total nursing interventions captured, 14 interventions accounted for 55.2% of the total, being the ranking as follows: vital signs monitoring (label is 6680) with 8.6% (n=244), surveillance (6650) with 5.9% (n=167), emotional support (5270) with 3.9% (n=110), neurologic monitoring (2620) with 3.7% (n=106), exercise therapy: ambulation (0221) with 3.7% (n= 105), fall prevention (6490) with 3.7% (n=104), positioning (0840) with 3.6% (n=102), active listening (4920) with 3.6% (n=102), documentation (7920) with 3.6% (n=102), health education (5510) with 3.2% (n=90), exercise promotion (0200) with 3.2% (n=90), pain management: acute (1410) with 3.2% (n=90), positioning: wheelchair (0846) with 3.1% (n=87), and bed rest care (0740) with 2.2% (n=61).
DISCUSSION
This study was conducted to identify and categorize the most prevalent stroke nursing interventions selected by Korean nursing students according to NIC system. Compared to previous studies [13] on nurse interventions, neurologic monitoring, vital signs monitoring, transport, documentation, surveillance, medication administration: intravenous, circulatory care: arterial insufficiency, order transcription, and pain management interventions showed a high frequency. These interventions were distributed in 6 domains (physiological: complex, physiological: basic, safety, health system) and 20 classes. It can be seen that nursing interventions chosen by nursing students reflect the various problems of patients in that they generally suffer from not only physiological disability but also psychological, social, and economic disability through a long rehabilitation period, although there were differences depending on the brain lesion, treatment period, and clinical progress. Interventions such as neurologic monitoring, vital signs monitoring, transport, documentation, and surveillance, which are essential for stroke patients, were frequently performed by both nurses [13] and students, but differences were also found. Invasive interventions such as intravenous medication administration, the frequency was remarkably low among students, which is considered to be a limitation of invasive interventions due to the background emphasizing patient safety, consent, and right to treatment. Instead, the students performed interventions such as medication administration (oral, skin), teaching: prescribed medication, and medication facilitation. Order transcription were not found, which is considered to be because it is an intervention that only nurses can perform.
Second, in general, heart disease increases with age and the risk of stroke increases accordingly. Whereas, it can be said that the possibility of cardiovascular disease in stroke patients is very high. It has been reported that stroke most often occurs within 2 weeks after acute myocardial infarction [17-19]. So, it needs to identify interventions by considering heart diseases in stroke care. In previous studies [20], physical comfort (including care of the activity, comfort, mobility, hygiene, skin, self-care, and nutrition), a specialist function, sustaining a safe environment, and strengthening the input of family were emphasized as the role of nursing. In addition, interventions were performed in the order of behavioral, physiological: basic, physiological: complex, and safety [20], which was similar to the domain distribution confirmed in this study.
Third, among the total of interventions performed by the students, the largest number of interventions (n=906, 32.0%) belonged to the physiological domain, which was subdivided into 6 classes: immobility management, activity and exercise, self-care facilitation, physical comfort promotion, nutrition support, and elimination management. Physiological: basic means care that supports physical functioning. It is considered that the performance of nursing interventions such as “immobility management”, “activity and exercise”, and “physical comfort promotion” in order to solve the limitation of body movement due to paralysis and the immobility, subluxation, genu recurvate, and muscular weakness problem was high due to the characteristics of patients with stroke. In previous studies related to the nursing process with stroke, physical mobility was identified as a priority nursing problem and diagnosis [21]. This is justified by the result that stroke is a neurogenic motor disease likely leading to damage of voluntary movement control. So, it can be seen that performance related to impairment of mobility appears as a priority intervention that must be provided [22]. According to the previous studies, the self-care problem after stroke is usually due to the cerebral hypoperfusion [23], and interventions related to self-care assistance also show the relation to motor aftereffects. Thus, considering that patients with stroke often have difficulties in self-care temporarily or for a long time due to these physical limitations, it is suggested that the performance of interventions such as “self-care facilitation” of the basic level was high. Also, nutritional imbalance often occurs due to dysmasesis and dysphagia in patients with stroke, it is considered that nutritional support was appropriately applied by students.
Fourth, 655 (23.2%) interventions belonged to the safety domain, which was included into 1 class: risk management (23.2%). Seven nursing interventions: 244 (8.6%) vital signs monitoring, 167 (5.9%) surveillance, 104 (3.7%) fall prevention, 100 (3.6%) 3 types of environmental management, and 40 (1.4%) risk identification were identified in the data. These interventions related to care activities that were mostly aimed at the implementation of interventions such as fundamental physical needs for patient safety. In the same context, students seem to be aware of the importance of potential preventive interventions as well as actual health problems. As awareness of patient safety such as surveillance, fall prevention, and risk identification increases, interventions also tend to increase [18], so if students are actively educated during clinical training, such as presenting best cases for patient safety, and using practical guidelines, it can be expected that they will exert more positive effects in practice.
Next, 644 (22.8%) interventions belonged to the behavioral domain, which were subdivided into 5 classes: 222 patient education (7.9%), 190 coping assistance (6.7%), 145 communication enhancement (5.1%), 45 psychological comfort promotion (1.6%), and 42 cognitive therapy (1.5%). The nursing students showed concerns for problems about the patient education, as a facilitator of personal recovery. This suggest that students in Korea are more focused on health education about the aspects of disease care, enhancement of coping, communication, and cognition for maximum recovery to the state before the onset of stroke. This is desirable direction of the performance of nursing interventions considering the background facts of previous studies [24,25] related to the performance of nurses in which that many nurses report about a lack of time for providing interventions related to patient and family education because of the heavy workload of physical care.
Finally, the most 10 frequent nursing interventions are more specific to the stroke patient. Of these, 10 high-ranking interventions were vital sign monitoring, surveil-lance, emotional support, and neurologic monitoring, and it is considered that these are the fundamental and critical interventions performed at all level of nursing and especially for patients with stroke.
CONCLUSION
Stroke can occur in all population, but it is a geriatric disease that comes along with aging, and the incidence and mortality rates are high in the older population. It is thought that the identification and categorization of specific nursing interventions for stroke patients will contribute to the standardization and quality improvement of gerontological nursing practice. These results are also helpful to clinical preceptors, as well as faculty in gerontological nursing academics, for the improvement of a standard curriculum for students and in evaluating the competency of students with regard to knowledge, attitude, and skills toward gerontological nursing. Additionally, an analysis of how these selected nursing interventions are similar to or different from to those of students in other universities or other countries, is necessary. If the interventions used were different from interventions selected by other students, an analysis including the differences in patient needs for healthcare and priorities should be conducted. Thus a comparison of the significance of nursing interventions should be surveyed internationally. Furthermore, since the data were collected from one university, it is difficult to generalize the characteristics of nursing interventions.
Notes
Authors' contribution
Acquisition of subject, Data analysis, Manuscript preparation- PJE.
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
Funding
None.
Data availability
Please contact the corresponding author for data availability.
Acknowledgements
This paper was supported by Research Funds of Kwangju Women's University in 2022 (KWUI22-049).