Nurses' management of older patients with post-anesthesia delirium: A Q methodology approach
Article information
Abstract
Purpose
This is an analysis of the experiences of nurses in Post Anesthesia Care Units (PACUs) in caring for older patients with emergence delirium using the Q-methodology.
Methods
The Q-methodology, which is used to explore and understand human subjectivity, was applied. Thirty nurses who had experiences in providing nursing for delirium in older patients after surgery in a PACU participated in this study.
Results
This study revealed three factors regarding the frame of reference of PACU nurses in detecting and managing older patients' emergence delirium: “detect the deviant changes leading to instability”, “focus on the patient’s degree of cognitive recovery within the framework of recovery time”, and “awareness of possible clues based on the patient’s underlying disease(s)”.
Conclusion
These findings are expected to be utilized as a basis for more practical and accessible PACU nurse delirium education that reflects nurses’ subjective viewpoints explained by the three identified factors.
INTRODUCTION
A common medical problem that occurs preferentially in surgical patients over the age of 65 is postoperative delirium [1,2]. Delirium is a real emergency that requires immediate professional attention and treatment [3]. Delirium that presents in post-anesthesia care units (PACUs) is called emergence delirium (ED), which can be attributed to the residual effects of general anesthesia and must theoretically be solved within minutes to hours [4]. Emergence delirium presented in 37.0%(339/915) of the patients during their PACU stays [5].
Delirium is a common complication in older patients after surgery [4,6]. According to its time of onset, delirium can be divided into emergence delirium (ED, in the immediate post-anesthesia period) and postoperative delirium (POD, usually within five postoperative days) [7]. It has been reported that ED during the first hour of tracheal tube removal is a predictor of delirium at five days after surgery [4]. Thus, delirium, which can occur extremely early during the anesthesia recovery period, can be used as an entry point for the initiation of interventions and the implementation of intensive strategic processes of delirium interventions [8]. Patients with ED had worse postoperative outcomes, including more pulmonary complications, longer hospital stays, and a high percentage of readmissions [5].
Studies have shown that PACU nurses are on the front line in managing emergence delirium in older adults after surgery [4,9]. If delirium is assessed regularly due to PACU nurses’ strategies for frequent contact, it can be monitored accurately as such frequent contact offers ideal opportunities to observe and record the characteristics of delirium symptoms [9,10].
As a common operative complication, POD can affect patients of all ages, especially aged patients (65 years and older), and most patients who develop delirium in 5 postoperative days have experienced ED. PACU is the key bridge between the operating room and hospital wards and, as such, is the first place where changes in patient condition are determined and treated [8].
Although studies have been conducted on the usefulness of the tools for early detection of delirium, delirium diagnosis is mainly clinical, requiring frequent observation and high awareness. Managing emergence delirium in a PACU is very dynamic, and practical knowledge must be put into action over a short period of time [11]. The indications of delirium among patients in the PACU should be considered an abnormal process during their recovery period. The medical team should also determine delirium indicators, integrate them into nursing measures, and provide corresponding feedback and suggestions while patients are being transferred to wards [8].
In clinical practice, particularly in PACU nurses’ detection and management of ED, their use of the practical knowledge they have acquired through clinical experience is very important. Post-anesthesia nursing plays an important role in the early detection and treatment of clinical deterioration after surgery and/or anesthesia. Concomitantly, the effectiveness of post-operative care is highly dependent on the accurate analysis and synthesis of patient data and on the quality of diagnostic decisions arrived at through clinical reasoning. Intuition based on clinical experience plays an important role in overcoming uncertainty about a patient’s prognosis in the clinical reasoning of anesthesia nurses [12].
In terms of practical knowledge, it is necessary to explore how PACU nurses use a clinical frame of reference in detecting and managing ED in older patients. Therefore, this is an analysis of the experiences of nurses in the PACU in caring for older patients with emergence delirium using the Q-methodology.
METHODS
Ethics statement: This study was approved by the institutional ethics committee of the affiliated university (KUIRB-2020-0053-01). Informed consent was obtained from the participants.
Q-methodology was applied to identify nurses’ frames of reference about PACU nurses’ detection and management of ED in older patients. Q-methodology is an integrated research methodology that combines the advantages of quantitative and qualitative research methods and is used to explore and understand human perspectives [13,14].
1. Study Process
The specific process of the Q-methodology is as follows: First, through interviews, we create a list of statements called the Q-population. Second, we develop a Q-sample, which is the final set of Q-statements from the Q-population. Third, the P-sample is set by selecting the participant(s) to sort the Q-sample. Fourth, the sorting of the Q-samples is done using a Q-sort table. Fifth, a factor analysis is performed using the PQ Method program (version 2.35; Peter Schmolck, formerly of University of the Federal Armed Forces in Munich, Germany), and finally the identified factors are labeled and interpreted.
2. Data Collection
1) Q-population
This step is for developing a list of statements that are representative of the broad viewpoints concerning a topic, which is called the Q-population [15]. Q-population development relies on a literature review and interviews, but in fact, more statements can be obtained through interviews than through a literature review [16].
The data collection period was from March 23 to 30, 2020. In order to develop a Q-population, convenience sampling was conducted. 10 nurses who voluntarily expressed their intention to participate in this study from among nurses working in the PACU at K University hospital in Seoul and nurses with experience in providing nursing for ED in older adults after surgery were selected as interviewees. The inclusion criteria for participants were: 1) nurses who provided direct nursing care in the PACU and 2) nurses who had experience in providing nursing for ED in older patients after surgery.
The first author, with more than 5 years of experience working in a PACU, conducted the interviews. The interviews were conducted face to face in a quiet environment in a hospital’s education room. After their consent was obtained, the 10 participants were interviewed 3 to 4 times for a period of 30 minutes to 1 hour during each interview. In order to prevent omission of any interview content and to increase the accuracy of data analysis, the interview contents were recorded and transcribed. The transcripts were checked for accuracy against the original audiotapes among all researchers. The questions for the in-depth interview were as follows:
“When screening older patients for delirium in the PACU, what do you identify as ED?”
“What personal experiences have you had with detecting ED in older patients in the PACU?”
“What is the most important part of detecting delirium in older patients in the PACU?”
“What personal know-how or procedures do you use to detect and manage ED in older patients in the PACU?”
“What kind of care do you perform after detecting the ED in older patients in the PACU?”
The interviews were conducted until it was judged that no more new statements could be derived and theoretical saturation was reached. The Q-population consisted of self-referent statements used by PACU nurses to describe how they detect and manage ED in older patients. The entire Q-population construction process was reviewed and confirmed by all researchers and classified into two major aspects: detecting and managing ED in older patients. Finally, 67 self-referent statements on detecting ED in older patients and 34 statements on managing the ED of older patients were selected, resulting in a Q-population comprising 101 statements.
2) Q-sample
The next step was to compact the list by clarifying the statements to reduce any ambiguity of meaning and to remove statements to eliminate repetition. The Q-sampling process is usually done by domain experts. In this study, the first author, a PACU nurse with more than 5 years of clinical experience and the corresponding author, an researcher who has done many studies using Q-methodology, independently performed and cross-checked each other’s work to identify repetitions of viewpoints and to eliminate redundancies. After both authors compared their work, disagreements were discussed and resolved with the third author, a researcher with experience in qualitative and Q-methodology research. Between 20 and 100 statements are recommended for a Q-sample [14]. For this Q-sample of nurses’ frame of reference on detecting, and managing ED in older patients, 34 Q-samples were selected, including 17 statements about how PACU nurses detect ED in older adults and 17 statements on how PACU nurses manage ED in older patients.
3) P-sample
The group of participants who classify Q-samples in a Q-study is called a P-sample [17]. Brown [15] recommends that 40 to 60 participants are suitable for most studies; however, some specific studies may require a much smaller number of participants. For selecting the P-sample, convenience sampling was conducted, and the same criteria for choosing the participants in the in-depth interviews were applied. The purpose of the study was explained to nurses who provide direct nursing care in PACU and have experience in caring for ED in older patients after surgery. A total of 30 nurses, including those who participated in the in-depth interviews for the Q-population, were recruited as the P-sample.
4) Q-sorting
Q-sorting was carried out from April 6 to 12, 2020. The sorting was conducted at a time that the participants felt comfortable, and the location was considered for the participants’ convenience, such as cafes and seminar rooms in a hospital. When reading the 34 Q-samples one by one, the P-sample were asked to classify them as disagree (-), neutral (0), or agree (+), depending on the perceived degree of agreement. The distribution chart was used for the forced quasi-normal distribution. After the P-sample finished the Q-sorting, the first author interviewed them regarding the statements they most agreed with and the ones they most disagreed with to explore their reasoning. The interview data were used for factor interpretation.
3. Data Analysis
For analyzing the 34 Q-statements, a PQ-method program (version 2.35; Peter Schmolck, formerly of University of the Federal Armed Forces in Munich, Germany) was used. Factor analysis was conducted using the component factor analysis and Z-score of each item. To determine the ideal number of factors, we selected the results we found reasonable by entering the number of factors based on eigenvalues of 1.0 or higher.
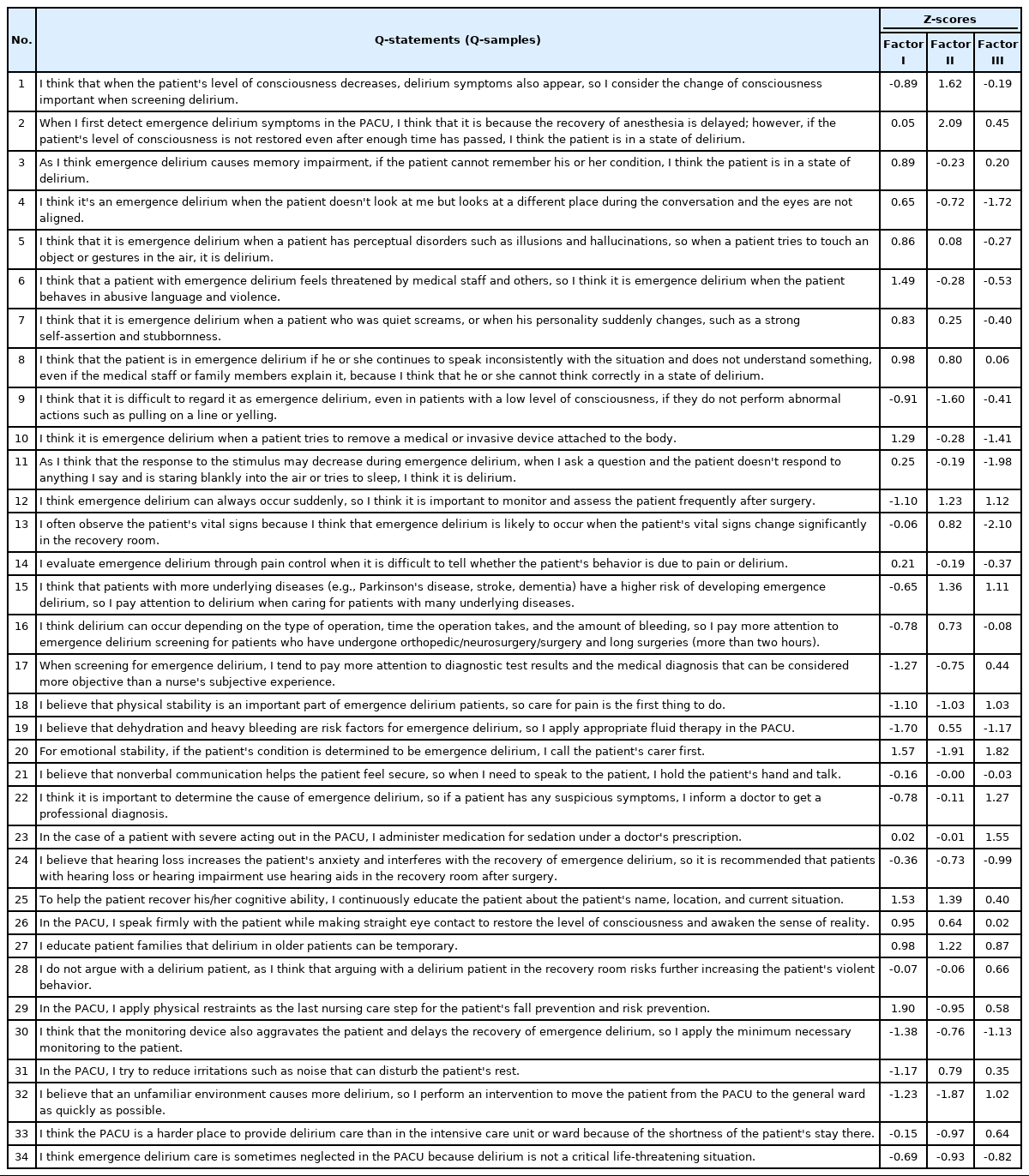
Factor naming was carried out centering on the items most agreed with (standard score 1.00 or higher) and the items most disagreed with (standard score -1.00 or lower) among the 34 items. To understand the characteristics of each factor, we referred to the interviews that showed a strong agreement or disagreement with a factor-specific P-sample, the reasons for strongly agreeing or disagreeing, and the typical characteristics and observations of representative P-samples during the interviews.
4. Ethical Considerations
This study was approved by the institutional ethics committee of the affiliated university (KUIRB-2020-0053-01). The researchers explained to the participants the study’s purpose and that the interview process would be recorded for analysis. The interview data were shared only among the researchers with protecting participants’ anonymity.
RESULTS
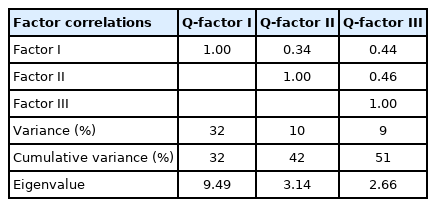
In this study, the factor analysis revealed three discrete factors that accounted for 51% of the total variance. The factors were “detect the deviant changes leading to instability”(32%), “focus on the patients' cognitive recovery pattern within the framework of the recovery time” (10%) and “aware of the possible clues based on the patients' underlying disease(s)” (9%). Since Factor I had 32% explanatory power, it can be viewed as the factor that most often explains the subjectivity of PACU nurses' ED detecting and managing after surgery. The correlation between the three factors is shown in Table 1. The correlation coefficient between Factor I and Factor II was 0.34, between Factor I and Factor III was 0.44, and between Factor II and Factor III was the relatively high correlation of 0.46 (Table 1). As Q-methodology focuses on discovering types without presupposing the complete independence of each type, controversy over the method of extracting factors due to high and low correlation coefficients is not raised.
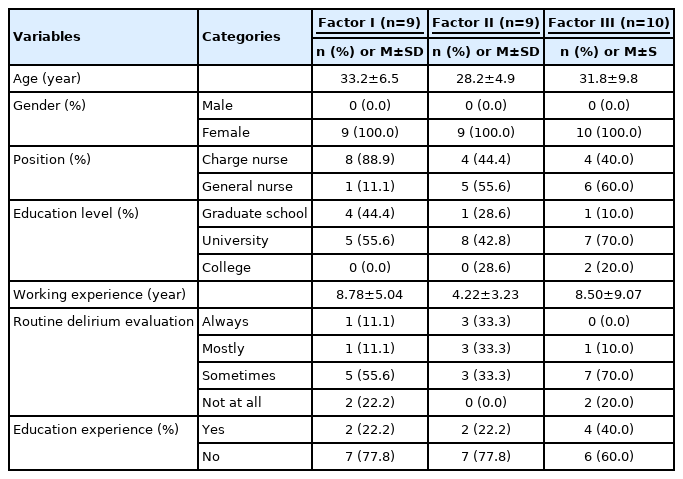
The demographic characteristics of the P-samples are shown in Table 2. Among the 30 P-samples, 2 P-samples were excluded from the results because they did not load significantly on a factor. The remaining 28 P-samples loaded on the three factors. The proportion of the factor is not important in Q-methodology as the purpose of Q-methodology is to identify the factors. Two general requirements for factor reliability that allow each factor to be considered to possess significance and powerful explanations are as follows: whether the number of loaded people is more than four and whether its eigenvalues of 1.0 or higher [14]. The factors identified in this study were statistically significant because all three factors had eigenvalues > 1: 9.49, 3.14, and 2.66, respectively.
Factor I. Detect the deviant changes leading to instability
Factor I was composed of 14 distinguishing Q-statements that nine participants loaded on. This factor agreed on Q-statements 20, 29, 25, 6, 8, 27, and 10 and disagreed with statements 30, 19, 9, 32, 34, 31, and 17 (Table 3).
The participants included in this factor prioritized physical and emotional stability in ED care and provided care for emotional and physical stability. Therefore, when it is thought that the patient's physical stability is threatened, the use of physical restraint is considered acceptable. They continually provide the patient with information about his/her name, location, and present situation in order to improve their cognition; if the patient continues to speak out of context, it is considered ED. These participants said they believe that the nurse’s rapid assessment of ED is necessary and that it is necessary to pay attention to patients, even if they do not behave abnormally.
The meaningful content of the interviews included:
When an old patient shows a subtle change out of normal, I am always paying attention to them because they are very likely to be physically injured due to sudden behavior. If it is determined that the risk of physical damage to the patient due to delirium is very high, physical restraints are sometimes provided to prevent physical injury.
Factor II: Focus on the patient’s cognitive recovery pattern within the framework of recovery time
Nine participants loaded on Factor II, which consisted of 13 distinguishing Q-statements. This factor agreed on Q-statements 2, 27, 25, 15, 1, and 12 and disagreed with statements 9, 32, 24, 34, 4, 20, and 30 (Table 3).
The participants included in this factor provide nursing care with an emphasis on restoring the patient’s cognitive function and through experience have become aware of when a patient should begin to recover consciousness after anesthesia. Based on this experience, the patient’s cognitive function is predicted in advance according to the time frame of recovery, and if the cognitive decline does not recover within the predicted time and persists, it is regarded as ED and delirium care is provided. Initially, the failure to return to normal is considered the effect of anesthesia, but when it is outside the predicted time frame, delirium is suspected. For these respondents, the range of time was an important reference point for judging delirium.
The meaningful content of the interview included:
Most patients come to the PACU right after surgery, so they cannot answer questions to check their level of consciousness because of the anesthesia. So, I think delirium is if the patient does not communicate well with the nurse and shows a low level of consciousness when the delirium evaluation is performed about 30 minutes after the patient comes to the PACU.
Factor III. Awareness of possible cues based on the patient’s underlying disease
Ten participants were included in Factor III, which was composed of 14 distinguishing statements. This factor agreed on Q-statements 20, 23, 15, 25, 12, 27, and 22 and disagreed with statements 13, 11, 30, 4, 34, 19, and 10 (Table 3).
Factor III assumes that ED can occur at any time in older adults and prepares care for ED as a top priority. Participants in this factor prepare to provide delirium care for patients who are expected to have a high probability of delirium, such as older adults by acquiring the patient's medical information in advance. Participants believe that there is a cause for delirium and that the especially, older patient's underlying disease(s) is one of the causes of delirium. They thus intend to acquire a record of the older patient’s underlying medical condition before the older patient comes to the PACU. Older patients with underlying disorders or comorbidities are more closely observed, and the participants begin to suspect ED when even subtle physical and psychological symptoms such as changes in vital signs, inconsistent eye contact, and increased irritability are noticed. In addition, this factor seeks to prepare for the older patient's delirium in advance through efforts such as waiting for a caregiver, preparing medication(s) in advance, and identifying and preparing for an underlying disease.
The meaningful content of the interview included:
I think first of which older patients are most likely to show delirium. For patients who are likely to show delirium, various preparations are made to prepare for immediate treatment. I think it’s a good method to consult with the doctor in advance and prepare drugs or physical restraints. I think that when a patient with suspected delirium symptoms enters the PACU, it is more efficient in many ways to diagnose it with a doctor than for the nurse alone to judge the patient’s condition. For the patient's prognosis, the early detection of delirium is important, and I think that appropriate treatment has to be provided.
DISCUSSION
From the findings, common traits shared by all three factors were for PACU nurses to confirm, compare, interpret, and predict that the older patients are presenting ED in the PACU. Factor I refers to the postoperative instability of older patients as a focal point of delirium [4] that PACU nurses need to resolve within minutes to 1~2 hours after surgery. Factor I specifically represents the intuitive knowledge of PACU nurses. That is, it is closely related to PACU nurses' perception of hyperactive delirium in older patients, who first classify the visible abnormalities seen in older patients. PACU nurses with this factor prioritizes physical and emotional stability and provides care to prevent patients’ potential danger, such as falls. They disagree with transferring the patient before his/her stability is ensured.
Factor II represents the frame of reference for PACU nurses. PACU nurses are looking for possible ED and the initiation of interventions for what may or may not appear as behavioral deviations in the PACU, but which may later occur in the general ward. This form of ED was likely to result in POD and ongoing complications, specifically cognitive and physical deterioration that eventually required long-term care [18]. In particular, factor II is a management pattern in which the detection and management of delirium alternate. In this factor, PACU nurses provide nursing care with an emphasis on the recovery of the patient's cognitive function. Routine ED monitoring in the PACU can be important since delirium at discharge from the PACU is likely associated with poorer than expected outcomes, such as more pulmonary complications, longer hospital stays, and a high percentage of readmissions [1,3].
Studies have emphasized that crucial for the development of delirium is the presence of predisposing factors in combination with an exposure to factors occurring during the acute treatment phase, such as surgery [6,9,19]. However, there are no studies examining how PACU nurses utilize the history of an underlying disease in older patients to assess ED in PACU settings. Factor III represents the frame of reference of PACU nurses actively seeking signs of delirium based on underlying disease(s) in older patients after surgery. It is similar to the pattern shown by nurses in the general ward or intensive care units (ICUs) when assessing older patients' delirium [20]. However, in a PACU, the patient is in the process of waking up from anesthesia after surgery, which is a different state from that of older patients assessed by general ward or ICU nurses. In addition, since PACU nurses cannot meet their patients before surgery, they may be unable to grasp their basic personal and medical information or characteristics as well as general ward or ICU nurses. However, Factor III recognizes that the history of underlying diseases such as dementia, Parkinson's disease, and stroke in older patients can affect the onset of delirium in the emergency room and thus should be considered by PACU nurses in the emergency treatment of older patients.
Research suggests that early detection and prompt management are the key elements of delirium management and that a lack of awareness of delirium is a very common problem in clinical settings [9,21]. For PACU nurses, the detection and management of ED is an interlinked nursing practice that must be done rapidly and routinely. For the relevance of nursing practice, the accurate detection of ED in older patients in a timely manner in PACUs is a cornerstone for preventing emergencies through appropriate interventions. However, it has been reported that when nurses assess delirium in older patients, they tend to rely more on common methods frequently used in clinical settings and opinions shared among peers than on the use of standardized assessment tools [22]. The study’s Q-methodology findings revealed three factors about how PACU nurses know what to do in post-surgery ED care for older patients. They do not suggest that a certain factor was dominant, but rather that all of the factors were important and should thus be used in combination to provide better delirium care in PACUs.
Implications of the study
The educational significance of the implication of the results is that it can be used for training new nurses in PACU. That is, the identification information of ED in older adults needs to include identifying visible patterns of delirium, classifying directions according to patient recovery, and using prior information on patients potentially related to delirium. The findings represent a key component of practical knowledge for nursing management of older patients with delirium after anesthesia. Therefore, these components can help research on the development of related practical assessment tools. The practical implication of the results of this study can be used as a framework for mutual sharing and improvement of PACU nurses’ practical knowledge and can be used as an initial step to develop an ED management protocol for older patients.
Limitations
This study uses an exploratory methodology, but the explanatory variance of the three factors found in this study is only 51%. Therefore, the subjectivity of PACU nurses involved in the management of delirium in older patients requires further exploration.
CONCLUSION
The findings can help advance a practical understanding of delirium detection in older patients from the perspective of PACU nurses. These findings are expected to be utilized as a basis for more practical and accessible PACU nurse delirium education that reflects the participating nurses’ subjective viewpoints as explained by three factors. At the same time, the focus of each factor can be merged to contribute to effective delirium management and related practices of PACU nurses.
Notes
Authors' contribution
Study concept and design - KM and CSO; Acquisition of subjects and/or data - KM; Data analysis and interpretation - KM, KEY, and CSO; Manuscript preparation: KM, KEY, and CSO.
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
Funding
None.
Data availability
Please contact the corresponding author for data availability.
Acknowledgements
None.